Surgical sperm retrieval - Mesa, Pesa, Tesa & Tese
These are the various techniques to obtain sperm from the epididymis or testis from men who have no sperm in their ejaculate (azoospermia). If the cause of the azoospermia is an obstruction, then the sperm retrieval procedure is usually simple and can be done under local anaesthetic with sperm being frozen for future use. If the cause is 'non-obstructive' then the procedure will be more complex and best results are achieved with microsurgical techniques.
Some men do not have any sperm in the ejaculate, but still produce sperm in their testes. In this case, sperm can usually be obtained using Surgical Sperm Retrieval (SSR). Sperm are produced in the seminiferous tubules in the testes, pass into the epididymis and then into the vas deferens. It is the vas deferens which is cut or blocked during a vasectomy – hence the name of the operation. If a man has a blockage in the vas deferens or in the epididymis outflow tract – from infection, vasectomy or even congenital absence of the vas – this is called ‘obstructive azoospermia’. It is nearly always possible to retrieve sperm from the epididymis or testis from these men.
Other men sometimes have sperm production in the testes but the number produced is too few for them to appear in the semen; this is called ‘non-obstructive’ azoospermia. In about 40% of men with non-obstructive azoospermia sperm can be retrieved for ICSI, but it can be difficult to predict who will have sperm and who will not. Occasionally there may be few sperm in the ejaculate sometimes but not at other times. Our embryologists can sometimes find sperm in the ejaculate even when a Community Pathology laboratory reports that there are no sperm present. We usually recommend at least two semen samples analysed by our embryologists before people think of moving on to SSR.
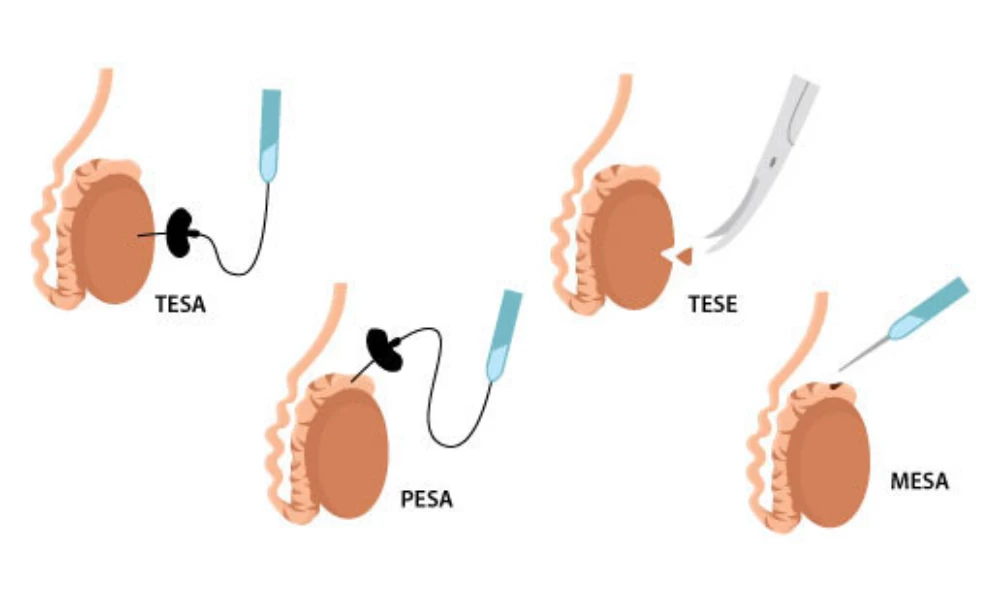
The testes and epididymis, and ways of retrieving sperm
Usually the two types of azoospermia can be distinguished by physical examination and a blood test for the hormone FSH. Occasionally a testicular biopsy can help make a diagnosis. Because a testicular biopsy carries some risks, whether to have a biopsy or not needs careful discussion with your doctor.
Even when a trial testicular biopsy produces no sperm, sperm can be found in 40% of these men if they try an ICSI treatment using SSR. This is because these men make sperm only in small areas of the testes, and it is a matter of luck whether the tissue taken at the trial testicular biopsy came from one of these areas.
Types of SSR
There are four types of SSR named after the techniques used:
- Microsurgical SSR: This is an operation done under general anaesthetic. The testis is removed from the scrotum and seminiferous tubules are examined under an operating microscope. This method reduces the risk of bleeding within the testis, and probably increases the chance of finding sperm with non-obstructive azoospermia by about 10%. It usually only used for men with nonobstructive azoospermia, particularly if the testes are small. The procedure is a lot more expensive than the other methods described below.
- PESA (Percutaneous epididymal sperm aspiration) refers to passing a fine needle through the skin into the epididymis.
- TESA (Testicular sperm aspiration) refers to passing a fine needle into the testes to aspirate seminiferous tubules from several areas within the testis.
- TESE (Testicular sperm extraction) refers to taking a larger amount of tissue from the testis through a cut in the skin.
Local anaesthetic usually gives sufficient pain relief for PESA, TESA and TESE procedures.
PESA, TESA and TESE are usually done well before the start of an IVF cycle. If sperm are found, they can be frozen and then thawed later for use on the day of egg collection. If we are not sure whether any sperm will survive freezing and thawing, we can thaw one straw from the sample one or two days after the SSR to test sperm survival. The number of straws needed to be thawed on the day of ICSI treatment will depend on the number and quality of the frozen sperm. Sometimes more straws have to be thawed than expected.
Risks and side effects of SSR
Nausea and loss of memory of the procedure are common side effects of sedative and narcotic drugs used during SSR.
If analgesic drugs are used during biopsy they will affect your ability to drive safely, so you need to arrange transport home from the clinic. You can not drive or use machinery during the next 24 hours, and we advise that someone remains with you for six hours after the procedure.
The drugs used for testicular biopsy can reduce the amount of air you breathe and thus the oxygen in your blood. If your oxygen saturation falls too low the doctor will stop the procedure and give oxygen. Very rarely you may require emergency drugs. Brain damage and death are theoretically possible, but so rare that no figures are available.
Bleeding and infection are possible complications of PESA, TESA and TESE, although they are rare. It is not uncommon to feel discomfort for several days, especially if TESE has been performed, and good scrotal support and Panadol is advised. If pain persists or recurs two or three days later, contact the clinic. TESA and TESE are likely to cause inflammation in the testis that could reduce future sperm production. They can also damage blood vessels. Up to 80% of men having TESE will have inflammation or collection of blood (called a bruise, or haematoma) at the site of the biopsy.
Complete loss of blood supply and atrophy of the testis has been reported after a TESE procedure. A repeated TESE procedure is more likely to be successful if it is done at least six months after the last procedure, to allow the testis time to recover from temporary damage. Similar damage on a smaller scale may occur after TESA.


